PGCert Clinically Enhanced Non-Medical Prescribing
Course details
Year of entry
2026
Duration
1 YR (PT)
Institution Code
G53
Location
Wrexham
Why choose this course?
This course combines the Independent/Supplementary Prescribing qualification with advanced clinical skills training. Unlike a standalone prescribing module, this enhanced pathway integrates physical examination, clinical reasoning and decision-making alongside the prescribing qualification.
You will:
- Gain the Independent/Supplementary Prescribing qualification on successful completion
- Develop enhanced clinical assessment skills to support safe prescribing decisions
- Learn in an integrated way, with clinical skills and prescribing running in parallel
- Improve your ability to deliver patient-centred, evidence-based care
Key course features
- The two modules run concurrently, providing a rich, practice-focused learning experience
- You will learn through a blend of taught sessions, campus-based simulation, supervised practice and self-directed study
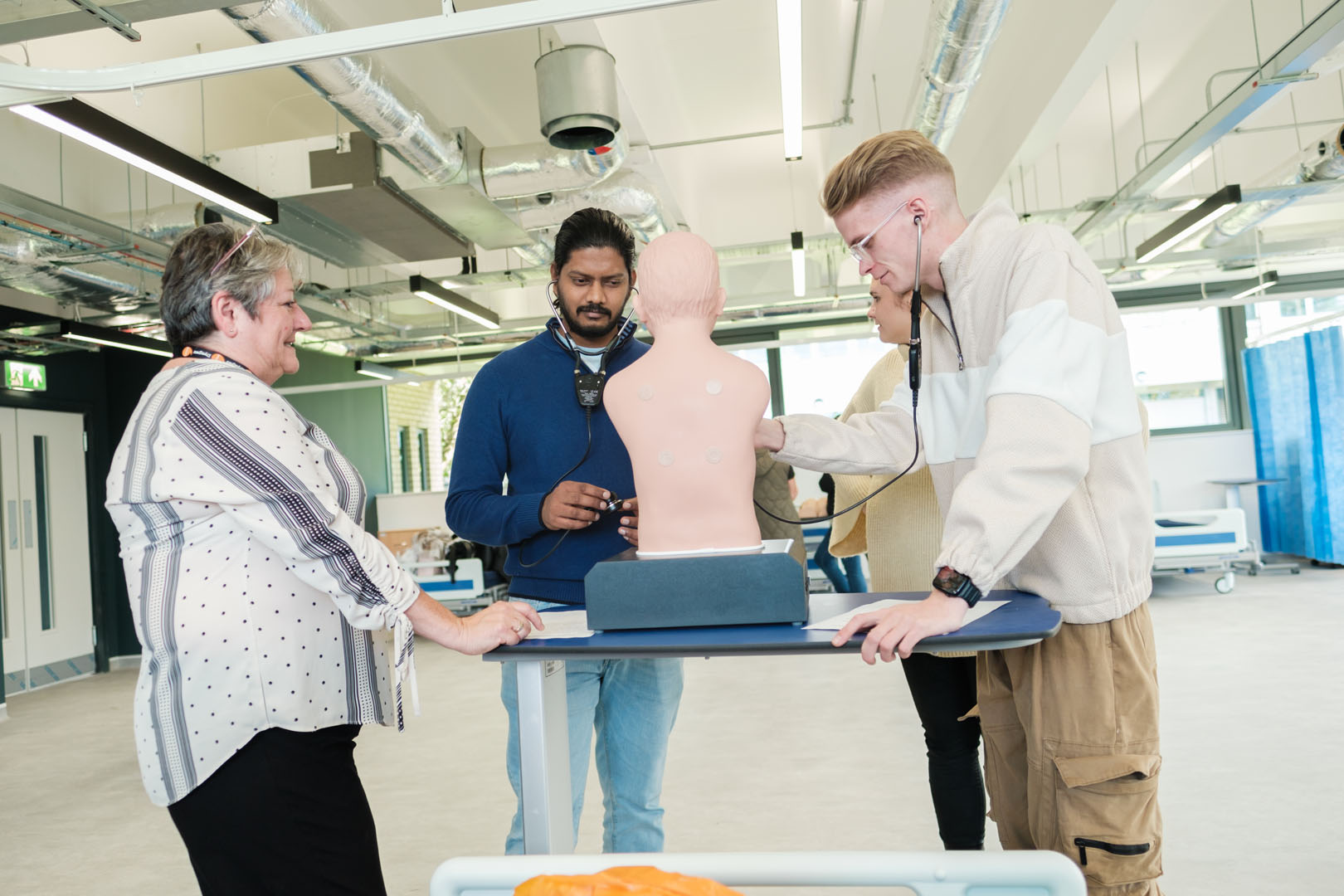
- Teaching draws on real clinical scenarios and use of the Healthcare Simulation Suite, giving you the opportunity to apply theory in a safe and supportive environment
What you will study
- Clinical Assessment, Diagnostics and Reasoning Part 1: In this module, you will develop the knowledge and skills needed to carry out safe and effective prescribing decisions. You will learn the principles of physical examination across the cardiac, respiratory, neurological and abdominal systems, and practise clinical history taking using structured consultation models. You will refine your collaborative communication skills, including the use of SBARR for safe referral, and apply clinical reasoning, heuristics and deduction to generate differential diagnoses. You will also build confidence in interpreting clinical investigations such as blood tests, chest x-rays and electrocardiograms (ECGs). Alongside this, you will explore therapeutic interventions and strategies for health promotion, supporting patient-centred care. The programme introduces you to the four pillars of advanced practice and guides you in applying reliable evidence to inform prescribing decisions. By integrating assessment, reasoning and evidence, you will be equipped to make safe, ethical and effective choices in clinical practice.
- Independent/Supplementary Prescribing for Nurses OR Independent Prescribing for Pharmacists OR Independent/ Supplementary Prescribing for Allied Health Professionals: In this module, you will focus on developing the knowledge, skills and professional behaviours required to prescribe safely, effectively and responsibly. You will study the legal, ethical and professional frameworks that underpin prescribing and explore the factors that influence decision-making, including patient values, co-morbidities and polypharmacy. You will examine strategies for safe and cost-effective prescribing, adverse drug reactions, pharmacovigilance and risk management. You will also reflect on your role as a prescriber within the wider healthcare team, strengthening your understanding of accountability and collaborative working. Emphasis is placed on patient-centred care, shared decision-making and the public health implications of medicines use. By engaging with evidence-based practice and developing critical thinking skills, you will be prepared to design, monitor and adjust treatment plans that optimise outcomes while maintaining professional responsibility
Entry requirements & applying
- The applicant must hold a degree at 2:2 and above to study at level 7
- If the applicant does not have a degree, evidence of completion of a level 7 module is required to study at level 7
- Have written endorsement from their employer or sponsoring organisation identifying that applicants have an appropriate area of clinical practice requiring prescribing skills and that they have up-to-date clinical, pharmacological and pharmaceutical knowledge relevant to their intended area of practice
- An offer of a place on the Independent Prescribing programme is conditional upon a DBS disclosure being deemed satisfactory by Wrexham University
- All proposed Designated Prescribing Practitioner and Practice Assessors and Supervisors will have their professional registration practice status confirmed
- Complete a programme application form and WU Generic Application Form
- Complete a NMP Short placement educational audit form as part of the application process.
- All short listed applicants must attend an interview
Pharmacists:
- Applicants are registered as a pharmacist with the General Pharmaceutical Council (GPhC) or in Northern Ireland, with the Pharmaceutical Society of Northern Ireland (PSNI)
- Applicants are in good standing with the GPhC and/or PSNI and any other health care regulator with which they are registered
- Applicants must have an identified area of clinical or therapeutic practice in which to develop independent prescribing practice
- They must also have relevant clinical or therapeutic experience in that area, which is suitable to act as the foundation of their prescribing practice while training
- On application, applicants must have a designated prescribing practitioner (DPP) who has agreed to supervise their learning in practice for a period of at least 90 hours of learning in practice
- Opportunities are provided that enable NHS, self-employed or non- NHS employed registrants to apply for entry onto the approved prescribing programme
- Confirm that the necessary governance structures are in place (including clinical support, access to protected learning time and employer support where appropriate) to enable students to undertake, and be adequately supported throughout, the programme
- Applicant selected to undertake a prescribing programme has the competence, experience and academic ability to study at the level required for that programme
- The applicant must hold a degree in order to study at level 7
- On application, they must ensure that the Designated Prescribing Practitioner has training and experience appropriate to their role. The Designated Prescribing Practitioner must have agreed to provide supervision, support and shadowing opportunities for the student for a minimum of 90 hours of supervised practice, and be familiar with the GPhC’s requirements of the programme and the need to achieve the learning outcomes
- Satisfactory DBS check
AHP’s/Nurses:
- Applicant is a registered AHP, registered nurse (Level 1), registered midwife or Specialist Community Public Health Nurse (SCPHN) before being considered as eligible to apply for entry onto a NMC, HCPC or GPhC approved prescribing programme
- Opportunities are provided that enable all AHP, nurse (level 1), midwife or SCPHN registrants (including NHS, self-employed or non- NHS employed registrants) to apply for entry onto an NMC, HCPC or GPhC approved prescribing programme
- Confirm that the necessary governance structures are in place (including clinical support, access to protected learning time and employer support where appropriate) to enable students to undertake, and be adequately supported throughout, the programme
- Students who are requesting RPL for modules already studied prior to enrolling on the PGCert will be guided to complete the recognition of prior certificated learning (RPL) application for exemption form where relevant. RPL will be at the discretion of the Programme Leader who will assess if the module/ credits identified for RPL are relevant and current within the context of the PGCert in Clinically Enhanced prescribing. Students may be asked to provide additional evidence to support their RPL request such as transcripts of results/certificates
- Applicant selected to undertake a prescribing programme has the competence, experience and academic ability to study at the level required for that programme
- Applicant is capable of safe and effective practice at a level of proficiency appropriate to the programme to be undertaken and their intended area of prescribing practice in the following areas:
1.6.1 Clinical/health assessment
1.6.2 Diagnostics/care management
1.6.3 Planning and evaluation of care
- Nurse/midwife or SCPHN applicants for V300 supplementary/independent prescribing programmes have been registered with the NMC for a minimum of one year prior to application for entry onto the programme
- On application, students must ensure that the Designated Prescribing Practitioner and Practice Supervisor has training and experience appropriate to their role. The Designated Prescribing Practitioner and Practice Supervisor must have agreed to provide supervision, support and shadowing opportunities for the student for 78 hours of supervised practice for nursing and students registered with the GPhC and HCPC must complete a minimum of 90 hours learning in practice facilitated by their DPP/PE, and be familiar with the relevant NMC, HCPC and GPhC requirements of the programme and the need to achieve the learning outcomes
Self-employed or non - NHS employed registrant:
Pharmacists, nurses and AHP’s who work outside NHS settings where clinical governance systems may differ or may not be applied in the same way, must ensure they comply with requirements to demonstrate their competence to practice. Students will be required to show in their application form and provide written evidence at interview of:
- How they audit their practice
- Keep up to date with current guidance, and
- How they safeguard the patients in their care within a clinical governance framework
- Name and address of premises
- Provide information if the placement area is currently being reviewed or been recently reviewed by Health Improvement Wales (HIW) or Care Quality Commission (CQC)
- Provide evidence at interview of the necessary governance structures in place (including clinical support, access to protected learning time and employer support where appropriate) to enable applicant to undertake the programme
- Provide two references with the application (1 x academic and 1 x professional). A clinical reference must be provided to include professional registration number of the referee for confirmation
Teaching & Assessment
You will learn through a blend of taught sessions, campus-based simulation, supervised practice and self-directed study. Teaching draws on real clinical scenarios and use of the Healthcare Simulation Suite, giving you the opportunity to apply theory in a safe and supportive environment.
For Module 1, you will complete a 1,500-word critical reflection on case management, worth 100%. You will also undertake a four-stage OSCE during 60 hours of practice-based learning, supported by a professional portfolio that evidences achievement of learning outcomes.
For Module 2, your assessment will be based on a Practice Assessment Document. This includes your initial student profile, learning contract, record and reflection of practice hours, mid-point review, a Clinical Management Plan, service user and carer feedback, and achievement of RPS competencies. You will also complete a personal formulary and demonstrate competence through an OSCE. In addition, you must pass an unseen numeracy examination (100% pass mark) and an unseen examination of 20 MCQs/short answer questions (80% pass mark). Supervised practice requirements vary by profession: 78 hours for nurses, and 90 hours (12 days) for pharmacists and allied health professionals.
Teaching and Learning
We offer workshops and support sessions in areas such as academic writing, effective note-making and preparing for assignments.
Students can book appointments with academic skills tutors dedicated to helping deal with the practicalities of university work. Our student support section has more information on the help available.
In terms of particular needs, the University’s Inclusion Services can provide appropriate guidance and support should any students require reasonable adjustments to be made because of a recognised prevailing disability, medical condition, or specific learning difference.
Fees & funding
You do not have to pay your tuition fees upfront.
The fees you pay and the support available will depend on a number of different factors. Full information can be found on our fees & finance pages. You will also find information about what your fees include in the fee FAQs.
All fees are subject to any changes in government policy, view our postgraduate fees.
Apply Now
Please contact postregadmissions@wrexham.ac.uk for an application form.
